 A Norwegian study will research whether bacteria are responsible for some types of back pain.
A Norwegian study will research whether bacteria are responsible for some types of back pain.
It’s just an ordinary bacterium that we all have on our skin. But it keeps some people with herniated discs in severe and almost constant pain, according to researchers from the University of Southern Denmark.
Their study showed that almost half of the patients with herniated discs have this bacterium inside their intervertebral disc. The results also showed that a three-month regimen of antibiotics could in many cases stop the symptoms.
This discovery is “the stuff of Nobel Prizes,” according to the English neurologist Peter Hamlyn at University College London Hospital in a 2013 interview with The Independent. The “stuff” he was referring to was a Danish study published in the European Spine Journal.
The study attracted international attention, and the news did not take long to reach Norwegian patients with chronic lower back issues. Some of them had gone for years with no relief from the intense pain.
Deluge of patients
Oslo University Hospital has experienced a rush of patients who want antibiotics since this study was published, says research director Kjersti Storheim at the hospital’s Communication- and research unit for musculoskeletal disorders (FORMI).
The answer they get is no.
“We don’t change our guidelines based on the results of a single study. A lot of scientific discussions about the Danish study have taken place. We believe that this study needs to be verified,” says Storheim.
A living hell
Heidi Økland knows all too well what a living hell is like.
The 36-year-old has had lower back pain on and off since she was 21 years old. In 2003, a herniated disc was detected in her lower lumbar region. She managed to keep the pain in check somewhat with chiropractic treatment and exercise.
When the pain suddenly changed in the autumn of 2012, she implemented a more structured training program, because this had helped before. But this time, the pain was of a different dimension altogether.
An MRI scan revealed visible changes in the bone marrow, just off the vertebrae, called Modic changes. They are named after the doctor Michael Modic who first described them.
But other findings indicated rheumatism as a possibility, and Økland was therefore diagnosed with rheumatism.
The pain just grew more and more unbearable. Eventually, she was no longer able to walk. Going to work became impossible, even with accommodations.
“It felt like I had a knife stuck in my lower back that was there all the time. I had no break from the pain. I could hardly sleep. Just getting dressed in the morning hurt so much that I almost had to throw up,” Økland says.
She tried numerous medications and treatments, but they only helped briefly, a little or not at all.
“The only thing I wanted was help for the pain, to stay healthy and to start living my life again. And especially, to be a mother to my kids,” she says.
She was told not to be afraid of the pain, which she found both frustrating and provocative.
Began to google
When the pain did not relent, Økland began googling. She came across research describing Modic. She also found a Norwegian group on Facebook where other patients described the same symptoms as she had. She discovered she was not alone.
Through her contact with other patients, Økland learned about the Danish Modic study. She sent her MRI images to the Modic Clinic in Denmark. This is a private clinic that began to treat patients with antibiotics after the Danish study showed positive results of such treatment.
She heard from Denmark that she could benefit from this treatment, and at the same time a private back specialist in Bergen told her that she qualified for back surgery. After much deliberation, she chose the latter.
Økland said it was tough to go through this situation alone and to go against advice and recommendations given by public health services.
The Danish clinic has also opened a branch in Spain. Many Norwegian patients have travelled abroad to obtain this treatment.
Knows that patients go abroad
Storheim is quite aware that patients go abroad to receive this antibiotic treatment.
She says researchers are just as frustrated as patients are that they don’t better understand the reasons why people get back pain and how the pain can be treated.
This treatment option “is finally something concrete for the large group of patients with nonspecific lower back pain. For many years the main intervention has been a psychological approach, for lack of truly effective treatment options,” she says.
Norwegian study initiated
Storheim is heading a large Norwegian project that is setting up a study right now. This must replicate the Danish one exactly in order to verify its findings.
One group of patients will receive antibiotics for 100 days and another group will receive a placebo. Patients must have had disc herniation during the past two years and prolonged back pain.
The Norwegian study also wants to add a new element to what was done in the Danish study. Samples will be taken of all the patients to investigate the hypothesis that a bacterial infection underlies the Modic changes.
Then the researchers will study epigenetic changes that may indicate whether the patient has bacteria in the spinal column. Epigenetics studies how the body organizes our genes.
What about antibiotics use?
“It will take one and a half years for the first results from this study,” says Storheim.
If the Norwegian researchers show that the bacteria level goes down in the group receiving antibiotics, the results will confirm the Danish study. Only then will antibiotics be made available to Norwegian patients with chronic back pain.
That will be a happy day for many back patients. But it is also a huge dilemma for the researchers and society.
High antibiotics use threatens our world. Antibiotic resistance is one of the biggest enemies in today’s health care system.
Back pain is a very common ailment in the population. Treating this group of patients with a 100-day antibiotic regimen could become a public health problem.
Storheim admits that the study risks adding to the problem.
But she believes that they have to check whether the Danish study is really true. Not only for the sake of research, but because patients deserve it.
Still more uncertainty than certainty
At this point, what is known about Modic is more uncertain than certain, Storheim believes.
What is quite certain is that Modic changes can be seen as a shadow under or over a disc on your MRI.
One of the hypotheses is that skin bacteria – swirling around in the bloodstream and penetrating into one of the intervertebral discs – are to blame, and that this happens in the context of a herniated disc.
The discs normally remain closed, so any infection takes a long time to be cleared out. This may cause inflammation that results in intense and constant pain.
This hypothesis was the basis for the previously published Danish study and is also the basis for the Norwegian study.
Expensive surgery
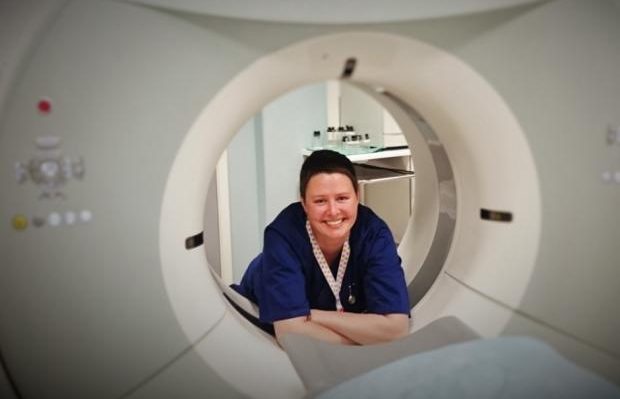
Økland had her back surgery in 2015. The operation was successful, and she is now back in a half-time position as a radiographer.
She is also some EUR 20 000 poorer, because her operation was private. The public health system deemed this type of operation an experimental treatment and therefore not advisable.
Økland has joined efforts to launch a separate diagnosis group for those with Modic changes under Ryggforeningen i Norge (Norwegian back association). Several of these patients have been to Denmark to receive antibiotics treatment. She understands them well.
“You become desperate when no one hears or believes you, and you’re not getting any help to deal with such intense, constant pain,” she says.
Wants knowledge-based treatment
Those who are establishing this association want treatment to be available in Norway. But it needs to be evidence-based, says Økland.
She believes it is time for Modic-related back pain to be defined as a specific type of back pain.
She says that although prolonged and sometimes severe back pain has been shown to accompany Modic abnormalities, not everyone with Modic changes experiences pain. A certain continuum probably exists, which complicates the picture and shows the need for a greater understanding of the underlying causes.
The help you get today is random, says Økland. Some Norwegian doctors are already prescribing antibiotics for their back patients, but many doctors are still reluctant to do that.
“The most important thing for us now is to increase the knowledge, interest and experience in the relevant disciplines. For that we require further research,” she says.
(sciencenordic)
